

updated April 17, 2025
Although I spend a lot of time talking about how to get pregnant, I’m also a big fan of conscious conception — having your baby at the right time for your family.
Some form of contraception is therefore necessary for many women, but most of the popular methods out there are hormonal birth control options, which work by shutting down your own hormones and manipulating your ovulation and menstrual cycle …
Which I’m obviously not a huge fan of.
There’s a common story that I hear time and time again in my practice:
A woman has less-than-desirable periods. Her menstrual symptoms affect her day to day life. Maybe she’s experiencing mood changes, pain, acne, PMS, breast tenderness, heavy bleeding, or any of the other myriad of symptoms that can go along with menstrual cycles.
↳ So, she goes to the doctor.
↳ She gets put on hormonal birth control to manage her symptoms.
↳ End of story.
It’s unlikely that there’s any follow-up or guidance on how long to stay on the hormonal birth control, or what it’s capable of doing to her body over the long-term.
A few years pass and she wants to come off of birth control, maybe to try to conceive, or maybe it just no longer fits into her lifestyle.
And she’s right back to struggling with those same initial symptoms — and often her fertility, too — which is usually what brings her to me.
Then we begin the process of healing her body, optimizing her fertility, and fixing all of the issues that hormonal birth control has created within her body.
Oof.
Knowledge is power.
It’s important to know ALL of the risks and potential side effects if you’re thinking about starting hormonal birth control (or, if you’re already on one). This way if you do decide to be on one of these forms of birth control, you’ll have made a fully informed decision and know what to look out for if issues come up.
In the United States:
〰 98% of women have used birth control at some point in their lives.
〰 62% of those of reproductive age are currently using hormonal birth control.
〰 the pill has been one of the most popular hormonal methods of birth control since 1982.
Birth control is prescribed for preventing pregnancy and to control acne, but also for a variety of fertility issues such as endometriosis, PCOS, ovarian cysts, pain associated with fertility issues, PMS, and irregular menstrual cycles.
While most people associate the term “hormonal birth control” with the pill, there are a variety of hormone-releasing birth control methods.

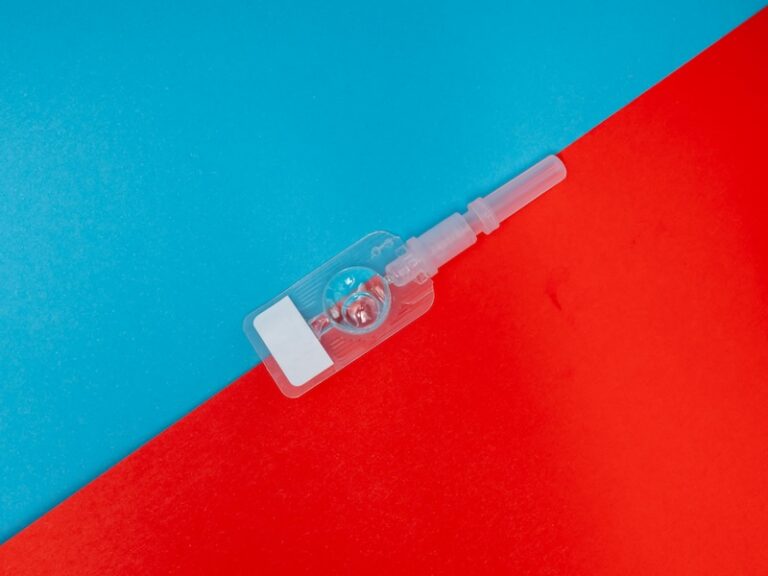
Nexplanon is a birth control implant that goes in the arm. This small, thin rod (about the size of a matchstick) is implanted under the skin of the inner, non-dominant upper arm by a healthcare provider.
The implant is made of ethylene vinyl acetate copolymer (plastic).
Nexplanon is made up of the following ingredients:
Note: while it’s not likely you’ll ovulate on Nexplanon, some studies show it is possible. However you’re still not likely to get pregnant due to points 1 and 2.
1 in 10 women stopped using Nexplanon because of an unfavorable change in their bleeding pattern:
Other frequent side effects that cause women to stop using Nexplanon:
Location and removal of the implant may be difficult or impossible because the implant is not where it should be. Special procedures, including surgery in the hospital, may be needed to remove the implant.
Implants have been found in the pulmonary artery (a blood vessel in the lung). If the implant cannot be found in the arm, your healthcare provider may use x-rays or other imaging methods on the chest.
Depo-Provera is a well-known brand name for medroxyprogesterone acetate, a contraceptive injection. It’s given as an injection every 3 months. Depo-Provera is 96% effective in preventing pregnancy.
Most women who choose the shot do it so that they don’t have to remember to take a pill every day. Other reasons:
Depo-Provera contains progestin.
Common side effects include:
After stopping Depo-Provera, it may take 10+ months before ovulation begins again. This is important to know if you plan on getting pregnant in the near future.
Use of Depo-Provera may cause you to lose calcium stored in your bone and decrease your bone mass. The longer you use Depo-Provera CI, the greater your loss of calcium from your bones. Your bones may not recover completely when you stop using Depo-Provera.
If you use Depo-Provera continuously for more than 2 years, it may increase the risk of weak, porous bones (osteoporosis) that could increase the risk of broken bones, especially after menopause.
You should not use Depo-Provera for more than 2 years unless you cannot use other birth control methods.

The NuvaRing contains the same kind of hormones found in certain combination birth control pills and they work the same way to prevent pregnancy, they are just administered differently.
Like the Pill, NuvaRing stops communication between your brain and ovaries, therefore stopping ovulation and the hormone fluctuations that come with it.
NuvaRing has been shown to be 98% effective.
NuvaRing is made up of the following ingredients:
Once NuvaRing is placed in the vagina, it releases a continuous low dose of hormones: 0.120 mg etonogestrel + .015 ethinyl estradiol per day.
The ring is worn in the vagina for 21 days, taken out for one week, and then replaced with a new one.
Common side effects include:
Serious side effects include:
NuvaRing may cause serious side effects, including blood clots.
Do not use NuvaRing if you smoke cigarettes and are over 35 years old. Smoking increases your risk of serious cardiovascular side effects from combination hormonal contraceptives, including death from heart attack, blood clots, or stroke.
First and foremost, getting in tune with your cycle, recognizing your fertile cues to know exactly WHEN you’re ovulating (and therefore very fertile) is my top recommendation.
How To Increase Cervical Fluid To Get Pregnant is a great resource that details what to look for to confirm ovulation — in order to get or prevent pregnancy.
The Natural Cycles app uses a unique algorithm that combines specific fertile cues such as your basal body temperature (your temp taken first thing in the morning before you get out of bed), your personal cycle fluctuations, LH hormone tests, and even the survival rate of sperm to give you “green days” — when you’re highly unlikely to conceive — and “red days,” when you’ll want to abstain or use protection.
Natural Cycles is the only FDA-cleared non-hormonal, non-invasive birth control app that syncs with your Apple watch or Oura ring.
For those of you with irregular cycles, chronic anovulatory cycles or another issue that prevents your cycles from being reliable, my top pick would be the Hormone-Free Copper IUD — it’s the only non-synthetic hormone based IUD! It promotes normal, healthy ovulation, meaning that it doesn’t suppress ovulation and you experience real periods.
Read more about the Hormone-Free Copper IUD.
One disadvantage of simply tracking your cycle or an IUD is that while they can keep you from getting pregnant, they won’t give you protection against STDs. A barrier method — like condoms — is still the best for both birth control and STD protection, but the kind you choose matters!
Many condoms contain synthetic fragrances, flavors, spermicides, and even carcinogenic chemicals. You don’t want any of that stuff near the delicate skin of your vagina!
Condoms don’t require the use of a spermicide, and are just as effective (in some cases more effective) as other barrier methods.
Although they’re technically non-hormonal, I’m not a fan of diaphragms and cervical caps or sponges because they both require the use of spermicide to be effective. Spermicides contain chemicals that are hormone disruptors, and can cause vaginal irritation and urinary tract infections. In fact, the most common chemical in spermicides, nonoxynol-9, is widely known to cause vaginal irritation.
There are so many effective and convenient non-hormonal contraceptives on the market, there truly is no need to use hormonal birth control, especially considering the slew of negative side effects associated with methods that use synthetic hormones to mimic your natural menstrual cycle.
There are many forms of hormonal birth control on the market, and they ALL contain synthetic hormones that throw off your natural hormonal balance.
Long term use of hormonal birth control affects not only your overall health, but can have lasting negative effects on your fertility health as well.
Trying a non-hormonal method of birth control is an important way to preserve your fertility AND your health until you’re ready to conceive.
While most people associate the term “hormonal birth control” with the pill, there are a variety of hormone-releasing birth control methods — nexplanon (implant), depo-provera (shot), nuvaring (insert), among others.
In the United States:
〰 98% of women have used birth control at some point in their lives
〰 62% of those of reproductive age are currently using hormonal birth control
〰 the pill has been one of the most popular hormonal methods of birth control since 1982
First and foremost, getting in tune with your cycle, recognizing your fertile cues to know exactly WHEN you’re ovulating (and therefore very fertile) is my top recommendation.
My favorite option is the Natural Cycles app, but you can also use a copper-free IUD!
The Fertility Code is the best-kept secret of women who want to take the guesswork out of conceiving, and give themselves every possible chance of getting, and staying, pregnant successfully.
Bringing together a personalized & custom approach, evidence-based information, science-backed protocols, and nurturing practices, this course is for anyone who is struggling to get pregnant, or thinking about getting pregnant soon. The course is a one-stop-shop for getting your body, mind and soul prepared for conception.
In less than 3 months, you will learn exactly what you need to do now to get pregnant successfully and have a healthy full term pregnancy with The Fertility Code.
Sarah Jane Sandy is a certified nutrition therapist, and a fertility and women’s health expert. She has helped hundreds of women increase their fertility naturally and go on to have healthy full-term pregnancies. She has been working with women and couples trying to get pregnant for over 16 years and over 90% of the women who work with her get pregnant and have healthy babies.
She also works with women trying to fix their hormone imbalances, as well as supporting women through pregnancy and the postpartum period. Learn more about her own fertility and hormone journey here. To send Sarah a message, complete her Contact Form.

Curious about your fertility health? Take this simple quiz to find out what factors may be harming your fertility, and learn what you can do about it!