

Feeling moody, bloated, tired, forgetful or just “off” lately? You might be wondering the same thing many women ask:
“Are my hormones out of balance, or am I just stressed?”
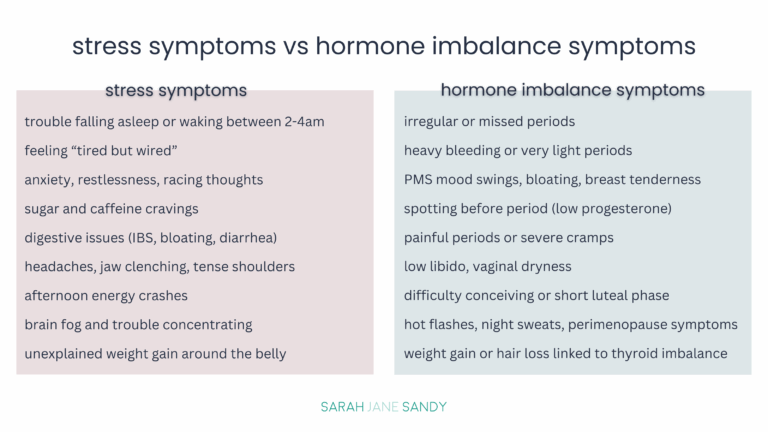
The tricky part is that hormone imbalance symptoms and stress symptoms often overlap — and oftentimes, stress actually causes the hormone issues. Understanding the difference is key for anyone navigating fertility challenges, PMS, perimenopause, or general hormone health.
When you experience stress, your adrenal glands release cortisol (your main stress hormone). A short spike in cortisol is normal, but when it stays high for too long, it can throw your whole system out of balance.
Cortisol is often called your “stress hormone,” and for good reason — it’s released by your adrenal glands any time your body perceives stress (physical, mental, or emotional). A quick burst of cortisol is healthy — it helps you wake up in the morning, get out of bed, and even power through workouts.
But when cortisol stays high for too long (think ongoing stress, lack of sleep, overexercising, or skipping meals), it can throw off the delicate balance of your other hormones.
Here’s how cortisol impacts your hormonal health:
Cortisol is not the enemy — but when it’s constantly elevated, it throws your progesterone, estrogen, thyroid hormones, and even insulin out of sync. That’s why stress management is one of the most underrated yet powerful tools for balancing hormones and supporting fertility.
Hormones are your body’s chemical messengers and when they’re in balance, everything flows smoothly. But even small shifts in estrogen, progesterone, thyroid hormones, or androgens (like testosterone) can cause ripple effects that show up in your cycle, fertility, mood, and energy.
Here are two of the most common ways women notice hormone imbalance in their daily lives:
Your menstrual cycle is like a monthly report card for your hormones. If something’s off, your period will usually tell you.
Signs of hormone imbalance in your cycle include:
In short: if your period feels unpredictable, overwhelming, or drastically different from month to month, it’s often your hormones waving a red flag.
Hormones also play a huge role in fertility and life stage transitions like PMS and perimenopause.
Whether you’re trying to get pregnant, managing monthly PMS, or moving into perimenopause, these symptoms often point back to hormone imbalance.
Stress and hormones are like two sides of the same coin. A little stress here and there? Totally normal. But when stress becomes chronic, it directly impacts your reproductive and metabolic hormones, making it harder to feel balanced, maintain energy, and even conceive.
When your body perceives stress — whether from work deadlines, poor sleep, intense exercise, skipping meals, low quality food, or emotional strain — it releases cortisol, your main stress hormone. In the short term, cortisol helps you adapt. But when cortisol levels stay elevated for weeks or months, it creates a hormonal domino effect:
Chronic stress doesn’t just make you feel frazzled — it literally pulls your reproductive and thyroid hormones out of balance.
You’ve probably heard the term adrenal fatigue — and while it’s not a formal medical diagnosis, it describes what many women experience when their stress response system gets worn out.
Signs of adrenal fatigue may include:
When your adrenals are overworked, your reproductive health takes a hit. Here’s how:
Your adrenal health and reproductive health are intimately connected. If you’re constantly in “fight or flight” mode, your body will naturally deprioritize fertility and hormone balance in favor of survival.

Because stress and hormone imbalance symptoms overlap so much, it’s easy to feel confused. The good news? Your body leaves clues. With a little self-tracking and reflection, you can start to see whether your symptoms are more tied to stress overload, hormone imbalance, or a mix of both.
Your menstrual cycle is one of the best tools for understanding your hormone health. By tracking your cycle, you can spot patterns that reveal whether your symptoms are cyclical (hormones) or more random (stress).
What to track:
If your symptoms line up with your follicular phase, ovulation, or luteal phase, it’s a strong sign your hormones are the driver.
If your symptoms pop up randomly — especially after stressful events, travel, poor sleep, or work deadlines — they may be more stress-related.
Sometimes, it helps to pause and check in with a few simple questions:
When do my symptoms show up?
How long have I been feeling this way?
Do my symptoms improve with rest, relaxation, or stress management?
Am I also experiencing changes in my menstrual cycle or fertility?
Could it be both?
Many women find stress is the trigger that worsens hormone imbalances they already have. If symptoms flare during stressful times and cycle phases, it’s likely a combination.
Bottom line: Cycle tracking and mindful self-reflection can give you major insight. You don’t need to guess — your body is already giving you data.

Balancing hormones isn’t about quick fixes — it’s about building small, supportive daily habits that lower stress and give your body what it needs to thrive. Here are some natural ways to calm cortisol, rebalance your hormones, and support fertility, energy, and mood.
Your daily routines play a huge role in how much cortisol your body produces. Lowering stress hormones doesn’t always have to mean big changes — often just a few intentional tweaks can make a significant difference:
Remember: lowering cortisol is not about doing less — it’s about doing the right things at the right time.
What you eat directly impacts both stress levels and hormone balance. Think of food as fuel and medicine.
Foods that support hormone balance:
Supplements worth considering:
Pairing nutrient-dense foods with targeted supplements can be a game changer for women struggling with hormone imbalance symptoms.
Some habits work like double-duty magic — calming your stress response and directly supporting hormone balance:
Bottom line: You don’t have to overhaul your life to see changes. Small shifts — like balanced meals, magnesium before bed, gentle exercise, and consistent self-care practices — can dramatically improve both stress resilience and hormone balance over time.

If you’ve been wondering for months (or even years) whether your symptoms are stress, hormone imbalance, or both — and nothing you’ve tried seems to help — it may be time to get professional support. While lifestyle changes are powerful, sometimes you need deeper insights into what’s really going on with your hormones.
Conventional bloodwork can give a snapshot of hormone levels, but functional testing often goes deeper by showing patterns over time and revealing how stress is impacting your reproductive system.
Common testing options include:
Functional testing helps connect the dots between your symptoms and the underlying imbalances — giving you a clearer map toward healing.
Sometimes, the most powerful step is not just knowing what’s off, but having someone educate and support you as you bring things back into balance. That’s where working with a functional nutritionist can make all the difference.
Benefits of professional support include:
If your symptoms are interfering with daily life, fertility goals, or your emotional wellbeing, professional support isn’t just helpful — it’s a game changer.
When it comes to your health, it’s not always either stress or hormones — the two are deeply connected. Chronic stress raises cortisol, which can throw off your progesterone, estrogen, thyroid hormones, and even your fertility. At the same time, hormone imbalances often show up through your cycle, PMS, or perimenopause symptoms, making it tricky to tease apart what’s really going on.
Here’s what to remember:
The good news? You can take back control. By tracking your cycle, lowering cortisol with daily habits, nourishing your body with hormone-supportive foods, and leaning on mind–body practices, you give your system space to reset. And if symptoms persist, functional lab testing and professional guidance can uncover the root cause and give you a personalized roadmap back to balance.
Yes. Chronic stress raises cortisol, your body’s main stress hormone. Over time, high cortisol can disrupt estrogen, progesterone, and thyroid hormones — leading to irregular cycles, PMS, fertility struggles, or even perimenopause symptoms showing up earlier than expected.
Early signs of hormone imbalance in women often include irregular or missing periods, mood swings tied to your cycle, stubborn weight changes, low libido, hair loss, acne, or worsening PMS.
Look at timing and context. If your symptoms flare with stressful events (work deadlines, poor sleep, big life changes), stress may be the driver. If they follow a pattern around your menstrual cycle (ovulation, luteal phase, PMS), it’s likely a hormone imbalance. Often, it’s a mix of both.
Absolutely. Stress doesn’t cause infertility on its own, but it can interfere with ovulation, lower progesterone levels, and worsen sperm quality in men. Learning stress management techniques can significantly support fertility outcomes.
Lifestyle changes are powerful: balanced blood sugar, nutrient-dense foods, quality sleep, stress-relieving practices like yoga or breathwork, and targeted supplements such as magnesium and B vitamins. For more personalized support, work with a fertility nutritionist or practitioner who can guide you through hormone testing and tailored strategies for your body and your needs.
The Fertility Code is the best-kept secret of women who want to take the guesswork out of conceiving, and give themselves every possible chance of getting, and staying, pregnant successfully.
Bringing together a personalized & custom approach, evidence-based information, science-backed protocols, and nurturing practices, this course is for anyone who is struggling to get pregnant, or thinking about getting pregnant soon. The course is a one-stop-shop for getting your body, mind and soul prepared for conception.
In less than 3 months, you will learn exactly what you need to do now to get pregnant successfully and have a healthy full term pregnancy with The Fertility Code.
Sarah Jane Sandy is a certified nutrition therapist, and a fertility and women’s health expert. She has helped hundreds of women increase their fertility naturally and go on to have healthy full-term pregnancies. She has been working with women and couples trying to get pregnant for over 16 years and over 90% of the women who work with her get pregnant and have healthy babies.
She also works with women trying to fix their hormone imbalances, as well as supporting women through pregnancy and the postpartum period. Learn more about her own fertility and hormone journey here. To send Sarah a message, complete her Contact Form.
© 2026 Sarah Jane Sandy. All rights reserved. Privacy Policy | Terms and Conditions |
Medical Disclaimer

Curious about your fertility health? Take this simple quiz to find out what factors may be harming your fertility, and learn what you can do about it!