

The health of a man’s fertility plays 50% of the role in conception and staying pregnant (yes, sperm issues can affect miscarriage too) yet there is so little support out there on how to properly evaluate male fertility.
I’ve compiled a checklist of everything that should be done when a couple is starting their preconception journey. I will cover how to test sperm and when, what to look for in a comprehensive semen analysis, which hormones should be tested, other markers that need to be looked at, and so much more.
This is for every woman, couple, and man who wants to be a parent someday!
What is preconception care?
Preconception care refers to the critical time BEFORE a couple actually conceives. When preparing for pregnancy, you want to begin intentional preconception care at least three months — but ideally 6-12 months — prior to starting the *trying to conceive* process. The life cycle of the egg and sperm is approximately 90-100 days, so everything you do (or don’t do!) in that window can affect the quality of the egg and sperm that will eventually meet.
Not only that, but intentional preconception care provides the opportunity for both of you to make changes that will improve your reproductive hormones and optimize the health of your entire body in preparation of making a baby. By improving the environment of the body, this directly results in the improvement of egg and sperm quality. Additionally, studies have shown that preconception care helps reduce the risk of miscarriage.
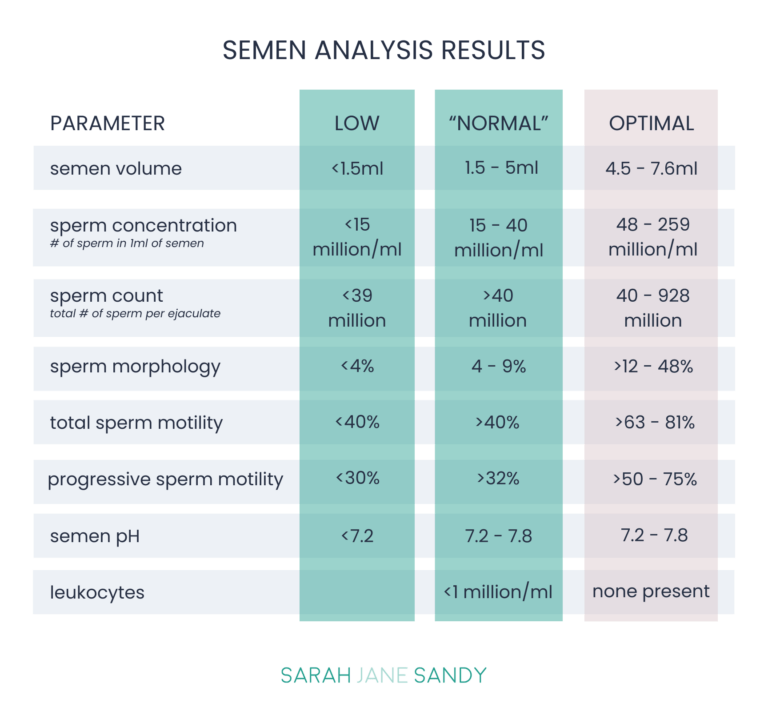
The most common male fertility test is called a semen analysis, also known as a “sperm count test.” It involves evaluating an individual’s semen and sperm. This analysis aims to determine the volume and characteristics of sperm, including essential factors vital for successful fertilization, such as sperm motility (movement), concentration (density), and morphology (size and shape).
Healthy sperm have a:
Tail: made of protein fibers, helps the sperm “swim” to the egg
Midpiece: the body/neck which contains the mitochondria, or energy source
Head: stores the nucleus and genetic material that may become a future baby
The total volume of semen which includes sperm and other ejaculate fluids (it isn’t just sperm). An adequate amount of semen is needed to deliver sperm in order for conception to occur.
This indicates how many sperm are in one milliliter of semen, essentially the density of sperm.
This is the total number of sperm in one ejaculate or semen sample. It is calculated by multiplying semen volume x sperm concentration = sperm count.
Refers to a sperm’s shape and structure, which greatly impacts fertilization and conception. The ideal morphology of a sperm includes a smooth oval head, well-defined acrosome (or cap), and a long tail with no visible abnormalities.
Refers to the sperm’s ability to move or swim efficiently, which is essential for unassisted conception.
Progressive motility is the percentage of sperm moving forward in straight lines (necessary for the sperm to reach the egg).
Non-progressive motility is the percentage of sperm moving, but not in a forward fashion (not good for fertility).
Total motility is the percentage of sperm moving, including progressive and non-progressive.
This is a marker of the acidity of the semen — sperm prefer alkaline (higher pH) versus acidic (lower pH) environments.
This is a test for white blood cells, a type of immune system cell. The presence of these indicate an infection that can negatively affect sperm and fertility.
In-Office Semen Analysis: The semen sample is collected in a small cup via masturbation (either at home or in the office) and is brought to the lab within 60 minutes. From there the lab will analyze the semen.
At-Home Semen Analysis: Similar to in-office analysis except the testing kit includes a buffering medium that keeps sperm alive for up to 48 hours, instead of 60 minutes. The sample is mailed in and the lab staff will analyze it.
My favorite male fertility test is the at-home sperm test from Legacy, with the sperm DNA fragmentation analysis added on.
The at-home sperm testing kit from Legacy allows you to understand your fertility with a comprehensive at-home semen analysis that tests all key metrics of sperm health. Just like a fertility clinic, but from the comfort of your couch. They also have the option to add sperm freezing. And you get results within 48 hours.
What’s included in the at-home sperm testing kit:
What’s included in your reports:
I always recommend adding on the sperm DNA fragmentation analysis to get a deeper understanding of sperm’s genetic health, and insight into what may be causing infertility, miscarriage, or failed fertility treatment(s).
This is a big one — if you want kids now, next year, or some day, test his sperm. It’s inexpensive, you can often do it from the comfort of your own home, and it gives you so much data to work with so you know where you’re starting from.
Here’s the thing about a couple’s fertility journey — there’s not usually an obvious physical abnormality that pinpoints the exact reason a couple is struggling to conceive. It could be him, it could be her, there’s no way to know without testing.
It’s easy to test — and usually treat — sperm health.
But it’s imperative to not just do a basic sperm count test — it’s really important to do a comprehensive semen analysis.
A basic sperm test will only look at sperm count, and if you’re lucky – motility, and morphology as well — but you need the data on so much more than that. There are a lot of other clues that we can get from a semen analysis that can tell us if something’s going on, making it essential to choose a comprehensive semen analysis that also looks at volume, pH, viscosity, WBC, and DNA fragmentation.
Ejaculate has more than just sperm in it — it has fluids from the prostate, bulbourethral glands, and all kinds of other juicy stuff that can tell us more about the quality of sperm than just count, motility, and morphology.
If his semen analysis indicates:
None of that information will come from a basic sperm test.
It’s imperative to follow the rules of sperm analysis. A man needs to be abstinent for at least three days prior to doing any kind of sperm testing. Abstinent means no ejaculation — no sex and no masturbation.
Why?
You’ll get a more accurate analysis by allowing your sperm to build up prior to testing, especially if you’re worried about sperm count.
It takes 72 days for the sperm to be made in the testicles, stored in the epididymis, and then ejaculated.
So whatever change he makes, whether it’s dietary, lifestyle, supplements, or environment, you need to wait a minimum of 72 days, but 90 days is ideal, to see the results of any changes made.
If his sperm count is less than 10 million, but especially less than 5 million, he needs a full physical exam and blood panel to look for blockages or genetic issues.
Here are just a few contributors to low sperm count:
Consider testing DNA fragmentation — a test that actually looks at the sperm itself to see if the DNA has been unraveled and damaged in some way — if dealing with unexplained infertility or recurrent miscarriages, or if you want to truly optimize the sperm quality to positively impact your future embryos and baby’s health.
An embryo is 50 percent of the female, 50 percent of the male — if he has a highly fragmented sperm, it’s not going to be capable of making healthy and viable embryos.
In addition to a comprehensive semen analysis, here is a list of bloodwork that I recommend all men get request from their doctor to evaluate their fertility health status:
The most common male fertility test is called a semen analysis, also known as a “sperm count test.” It involves evaluating an individual’s semen and sperm. This analysis aims to determine the volume and characteristics of sperm, including essential factors vital for successful fertilization, such as sperm motility (movement), concentration (density), and morphology (size and shape).
You can do a semen analysis both in a doctor’s office or from the comfort of your own home.
It’s imperative to follow the rules of sperm analysis. A man needs to be abstinent for at least three days prior to doing any kind of sperm testing. Abstinent means no ejaculation — no sex and no masturbation.
Why?
You’ll get a more accurate analysis by allowing your sperm to build up prior to testing, especially if you’re worried about sperm count.
If his sperm count is less than 10 million, but especially less than 5 million, he needs a full physical exam and blood panel to look for blockages or genetic issues.
Here are just a few contributors to low sperm count:
The Fertility Code is the best-kept secret of women who want to take the guesswork out of conceiving, and give themselves every possible chance of getting, and staying, pregnant successfully.
Bringing together a personalized & custom approach, evidence-based information, science-backed protocols, and nurturing practices, this course is for anyone who is struggling to get pregnant, or thinking about getting pregnant soon. The course is a one-stop-shop for getting your body, mind and soul prepared for conception.
In less than 3 months, you will learn exactly what you need to do now to get pregnant successfully and have a healthy full term pregnancy with The Fertility Code.
Sarah Jane Sandy is a certified nutrition therapist, and a fertility and women’s health expert. She has helped hundreds of women increase their fertility naturally and go on to have healthy full-term pregnancies. She has been working with women and couples trying to get pregnant for over 16 years and over 90% of the women who work with her get pregnant and have healthy babies.
She also works with women trying to fix their hormone imbalances, as well as supporting women through pregnancy and the postpartum period. Learn more about her own fertility and hormone journey here. To send Sarah a message, complete her Contact Form.



© 2026 Sarah Jane Sandy. All rights reserved. Privacy Policy | Terms and Conditions |
Medical Disclaimer

Curious about your fertility health? Take this simple quiz to find out what factors may be harming your fertility, and learn what you can do about it!